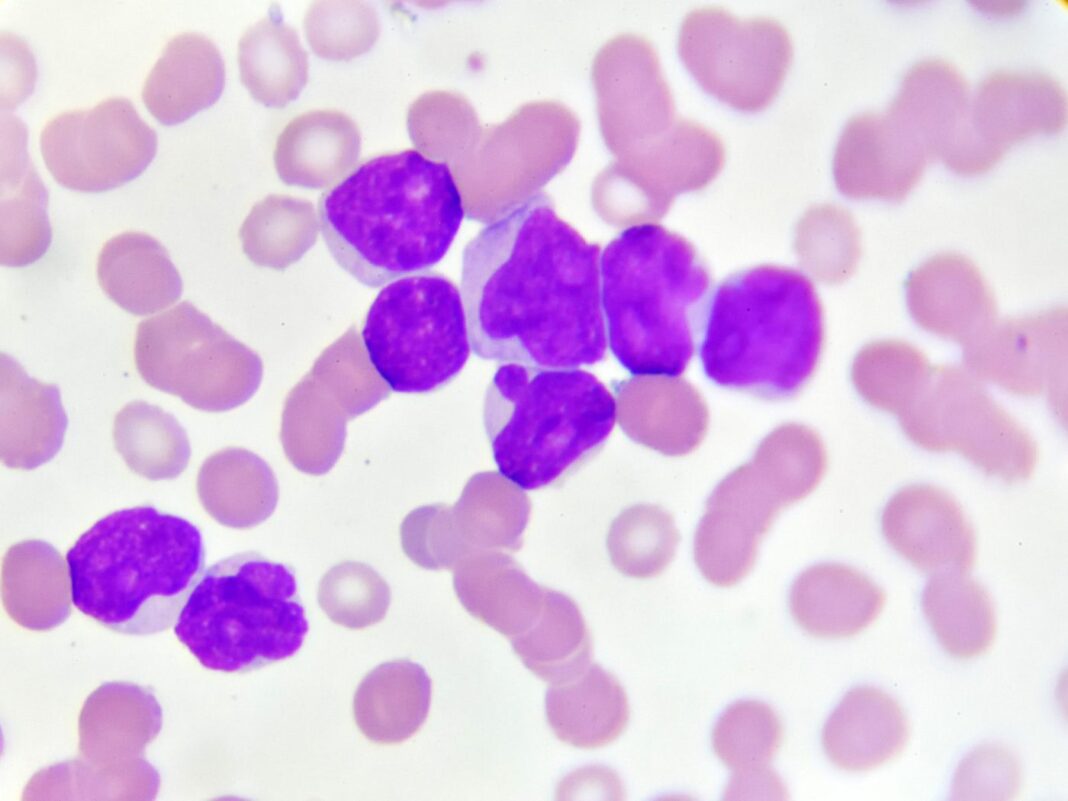
Acute myeloid leukemia (AML) starts in the bone marrow, but often quickly moves into the blood, as well. The main treatment for most types of AML is chemotherapy, sometimes along with a targeted therapy drug. This might be followed by a stem cell transplant. When AML relapses, it is more difficult to treat. Now, scientists at St. Jude Children’s Research Hospital report they have discovered a mutation in pediatric AML that physicians can use to identify high-risk patients and better guide treatment.
Their findings are published in the journal Blood Cancer Discovery in a paper titled, “Integrated genomic analysis identifies UBTF tandem duplications as a recurrent lesion in pediatric acute myeloid leukemia.”
The researchers evaluated the genomics of 136 St. Jude patients treated for relapsed AML.
“The genetics of relapsed pediatric AML has yet to be comprehensively defined,” wrote the researchers. “Here, we present the spectrum of genomic alterations in 136 relapsed pediatric AMLs. We identified recurrent exon 13 tandem duplications (TD) in UBTF in 9% of relapsed AML cases. UBTF-TD AMLs commonly have normal karyotype or trisomy 8 with co-occurring WT1 mutations or FLT3-ITD but not other known oncogenic fusions.”
“We started broadly because it was clear that we didn’t have a deep enough understanding about why kids with AML relapse in the first place,” said co-corresponding author Jeffery Klco, MD, PhD, St. Jude department of pathology. “We have a number of clinical trials at St. Jude for relapsed AML, so that gave us access to a large cohort of samples, and that is where the collaboration with our colleagues in computational biology became really beneficial to help us analyze the genetics.
“It became clear early on that there was a group of cases who had curious alterations in this gene UBTF, which had really only been superficially considered in the past,” Klco said.
UBTF-TD AML is more common in children than adults. It is also associated with poor outcomes and an increased incidence of minimal residual disease (MRD).
This mutation has been undetected in previous work. Researchers at St. Jude developed the computational approaches to identify this mutation, potentially in AML and other cancers.
“This is an extremely difficult mutation to detect, so a lot of work went into developing the right algorithms. We had to develop our method from scratch,” said co-corresponding author Xiaotu Ma, PhD, St. Jude department of computational biology. “Most of the existing methodologies assume there is only one event creating these kinds of mutations but, as with UBTF-TD, that isn’t always the case.”
“Now that we know what we’re looking for and how to find it, we can readily incorporate it into clinical genomics,” Ma said.
The findings pave the way for new strategies to target the protein created by UBTF-TD and to determine how the peptide contributes to leukemia.